Hydrocele is a prevalent condition that affects many men, causing swelling in the scrotum.
Understanding Hydrocele
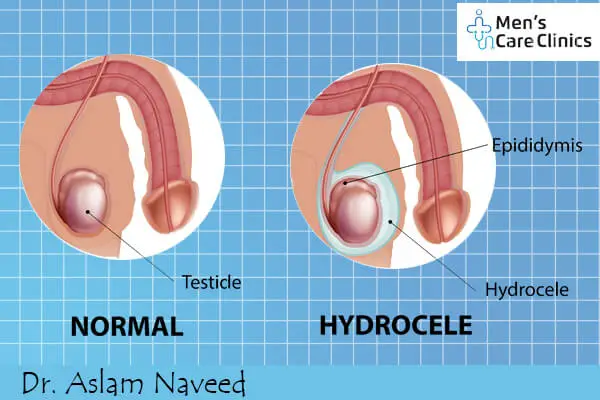
A hydrocele is a buildup of fluid in the scrotum, which is the sac-like structure that holds the testicles. This fluid buildup can lead to swelling, which may range from mild to more noticeable enlargement of the scrotum. Hydroceles can happen to anyone, but they happen most often to newborns and older people.
What Causes Hydrocele in Men?
Understanding the causes of hydrocele is essential for those affected and their Doctors. While hydroceles can develop for various reasons, the primary causes are as follows:
1. Processus Vaginalis Abnormalities: During fetal development, the testicles descend from the abdominal cavity into the scrotum through a small canal called the processus vaginalis. In some cases, this canal may remain open or partially open after birth, allowing fluid to flow into the scrotum and accumulate, resulting in a hydrocele.
2. Injury or Trauma: Physical trauma to the scrotum can lead to hydrocele formation. Injury or surgery in the scrotal area may disrupt the normal flow of fluid, causing it to accumulate and form a hydrocele.
3. Infection or Inflammation: If the testicles or structures around them are infected or inflamed, they can make the body make too much fluid, which can cause a hydrocele. Sexually transmitted diseases (STIs), epididymitis, or other health problems can lead to these infections.
4. Idiopathic Hydrocele: In some cases, the exact cause of a hydrocele may not be identifiable. This is referred to as idiopathic hydrocele, and it may occur without a clear underlying reason.
5. Other Medical Conditions: Certain medical conditions, such as hernias, tumours, or blockages in the spermatic cord, can disrupt the normal circulation of fluid in the scrotum, contributing to hydrocele development.
6. Lymphatic System Issues: The lymphatic system helps keep the body’s chemical balance. If there are issues with the lymphatic system’s drainage in the scrotal area, it can lead to the accumulation of fluid and the formation of a hydrocele.
Types of Hydrocele
Hydroceles can be categorized into two primary types: communicating and non-communicating. These distinctions are crucial for healthcare providers to determine the appropriate treatment and for individuals affected by Hydrocele to understand their condition better. Let’s delve into these two types:
1. Communicating Hydrocele: A communicating hydrocele is a type where there is a persistent connection between the scrotal sac and the abdominal cavity. This connection allows fluid to flow freely between these two spaces, resulting in the accumulation of fluid within the scrotum. Key features of communicating hydroceles include:
- Open Processus Vaginalis: During fetal development, the testicles descend from the abdominal cavity into the scrotum through a small canal called the processus vaginalis. This canal stays open in people with communicating hydroceles, letting fluid move between the belly and the scrotum.
- Fluctuating Size: One characteristic feature of communicating hydroceles is that their size can change throughout the day. They may be smaller in the morning and enlarge as the day progresses due to the accumulation of fluid from the abdominal cavity.
2. Non-communicating Hydrocele:
A non-communicating hydrocele, on the other hand, does not connect the scrotal sac to the abdominal region. Instead, it forms when fluid accumulates within the scrotum but cannot flow back into the abdominal cavity. Key characteristics of non-communicating hydroceles include:
- Closed Processus Vaginalis: In individuals with non-communicating hydroceles, the processus vaginalis typically closes during fetal development. This closure prevents fluid from freely moving between the abdomen and the scrotum.
- Stable Size: Non-communicating hydroceles often maintain a relatively consistent size throughout the day. Changes do not influence them in posture or activity, and they remain confined within the scrotal sac.
Hydrocele Symptoms
Understanding the symptoms and knowing when to consult a healthcare provider can help ensure timely diagnosis and appropriate care. Here are key hydrocele symptoms and when to consider medical evaluation:
1. Scrotal Swelling: The most noticeable symptom of a hydrocele is scrotal swelling. There is growth because fluid is building up in the scrotal sac. It may vary in size from mild to more noticeable enlargement.
2. Heaviness or Discomfort: Some individuals with hydroceles may experience a feeling of heaviness or discomfort in the scrotum, particularly when the swelling is pronounced.
3. Fluctuating Size: Swelling in patients with communicative hydroceles may enlarge and contract over the day. It might be smaller in the morning and enlarge as the day progresses due to fluid accumulation.
4. Transparency of Swelling: Hydrocele swelling is usually soft and can be transilluminated, meaning that when a flashlight is shined through the scrotum, the fluid-filled sac appears as a glowing, translucent mass.

When to Seek Medical Attention
While hydroceles are generally not associated with severe health risks, there are circumstances when seeking medical attention is advisable:
- Sudden or Severe Pain: Getting medical help right away is very important if you suddenly feel a lot of pain in your scrotum. Although pain is not a common symptom of hydroceles, it could indicate other conditions, such as testicular torsion, which require urgent evaluation.
- Rapid Swelling or Changes: If the scrotal swelling rapidly increases in size, becomes unusually large, or is associated with redness or warmth, consult a healthcare provider promptly. These changes could mean you have an illness or something else going on.
- Persistent Discomfort: If you have ongoing discomfort, pain, or a sense of pressure in the scrotum due to the hydrocele, it is advisable to consult a healthcare provider. They can evaluate whether intervention or treatment is necessary to relieve symptoms.
- Uncertainty About the Swelling: If you are unsure about the cause of scrotal swelling or have any concerns related to your genital health, seeking medical advice is a prudent step. Doctors can check out the person and do other tests to find out what is causing the swelling.
Diagnosis of Hydrocele
Diagnosing a hydrocele typically involves a combination of physical examination and, in some cases, imaging studies. Healthcare providers use these diagnostic methods to confirm the presence of a hydrocele, determine its type, assess its size, and rule out other potential causes of scrotal swelling.
Conservative Management of Hydrocele
In many cases, hydroceles, particularly non-communicating hydroceles, may not require immediate medical intervention. Conservative management, which includes monitoring and home care, is often a suitable approach. This approach allows individuals to observe the condition, assess any changes, and take steps to alleviate discomfort when necessary.
Surgical Options for Hydrocele Treatment
When conservative management approaches do not provide relief or when hydroceles become large, bothersome, or associated with discomfort, surgical treatment may be recommended. Surgery is considered an effective and definitive method for addressing hydroceles. Here are the primary surgical options for hydrocele treatment:
1. Hydrocelectomy
The most common surgery used to treat hydroceles is hydrocelectomy. During a hydrocelectomy:
- Anesthesia: As part of the process, a local or general anaesthetic is usually given to the patient to make sure they are comfy and not in pain.
- Incision: A small incision is made in the scrotum or lower abdomen, depending on the specific surgical approach chosen by the surgeon.
- Fluid Drainage: The surgeon carefully drains the accumulated fluid from the hydrocele, reducing the swelling.
- Removal or Repair: The hydrocele sac is either removed entirely or repaired, preventing the reaccumulation of fluid.
- Closure: To close the cut, medical pins or stitches are used.
Normally, hydrocelectomy is a safe, effective procedure with a low chance of problems. Recovery times are different for each person, but most people can go back to their normal lives within a few weeks.
2. Aspiration and Sclerotherapy
People who can’t have surgery or would rather have a surgical choice may think about aspiration and Sclerotherapy. This procedure involves:
- Aspiration: A needle is inserted into the hydrocele sac, and the fluid is withdrawn through the needle, reducing the swelling.
- Sclerotherapy: After draining the fluid, a sclerosing agent (usually a chemical solution) is injected into the sac to irritate its inner lining. This irritation promotes scarring and sealing of the sac, preventing further fluid accumulation.
Aspiration and Sclerotherapy are less invasive than hydrocelectomy but may have a higher chance of hydrocele recurrence. For best effects, you may need more than one session, and recovery is usually faster than after surgery.
3. Laparoscopic Repair
Laparoscopic Repair is a minimally invasive surgical option that may be recommended for communicating hydroceles, especially in children. During this procedure:
- Anaesthesia: The patient is put to sleep with general anaesthesia so they don’t feel any pain.
- Small Incisions: Several small cuts are made in the abdomen. After these cuts, a laparoscope (a thin, bendable tube with a camera on the end) and other surgical tools are put in.
- Identification and Closure: The surgeon identifies the communication between the abdominal cavity and the scrotum (the site of hydrocele formation) and closes it using sutures or other closure techniques.
Laparoscopic Repair offers the advantages of smaller incisions, reduced scarring, and potentially shorter recovery times compared to traditional open surgery.
4. Aspiration with Sclerotherapy (In Children):
For pediatric patients with hydroceles, aspiration with Sclerotherapy is often preferred due to its minimally invasive nature and the fact that pediatric hydroceles frequently resolve on their own. The procedure is similar to the adult version, but it is usually performed under local anaesthesia with sedation in children.
Prevention and Lifestyle Tips for Hydrocele
Hydroceles can sometimes develop without an identifiable cause, and there may not be specific measures to prevent them entirely. However, there are lifestyle tips and practices that can help reduce the risk of complications, promote overall scrotal health, and potentially minimize the likelihood of certain types of hydroceles. Here are some prevention and lifestyle tips:
1. Practice Safe Sex and STI Prevention: STIs (sexually transmitted diseases) can cause epididymitis, a condition that may make hydroceles more likely to happen. Having safe sex with protection methods like condoms and getting regular STI checks can lower the risk.
2. Avoid Trauma to the Scrotum: Trauma or injury to the scrotal area can increase the risk of hydrocele formation. Take precautions to protect the Scrotum during physical activities, sports, or work that may pose a risk of injury.
3. Maintain Good Genital Hygiene: Proper hygiene is essential to prevent infections that could lead to scrotal inflammation or other conditions associated with hydroceles. Keep the scrotal area clean and dry.
4. Promote Overall Health: Living a healthy life can improve your health in general, including the health of your Scrotum. Drink plenty of water, eat a healthy diet, work out regularly, and avoid drinking or smoking.
5. Address Groin or Abdominal Hernias: Hernias in the groin or abdominal area can sometimes lead to hydroceles, especially if there is a connection between the hernia sac and the Scrotum. If you think you might have a hernia or know you do, see a doctor to get it checked out and treated properly.
6. Early Detection and Treatment: If you notice any scrotal swelling or discomfort, seek medical attention promptly. Early diagnosis and appropriate treatment of conditions that can lead to hydroceles, such as epididymitis or inguinal hernias, can help prevent complications.
7. Care Instructions After Surgery: If you have surgery for a hydrocele, make sure you carefully follow the care instructions your surgeon gives you afterwards. This includes wound care, activity restrictions, and attending follow-up appointments to ensure proper healing and minimize the risk of complications.
8. Stay Informed: Please educate yourself about hydroceles, their risk factors, and associated conditions. This knowledge can help you spot possible signs and get medical help right away.